Comprehensive Overview of Bronchiectasis: Causes, Symptoms, and Treatment Options
This article provides an in-depth overview of bronchiectasis, covering its causes, symptoms, and management strategies. It explains disease progression, risk factors, and treatment options including medication and lifestyle care. Designed for a broad audience, it emphasizes the importance of medical consultation for accurate diagnosis and ongoing management of this lung condition.

Understanding Bronchiectasis: Key Facts
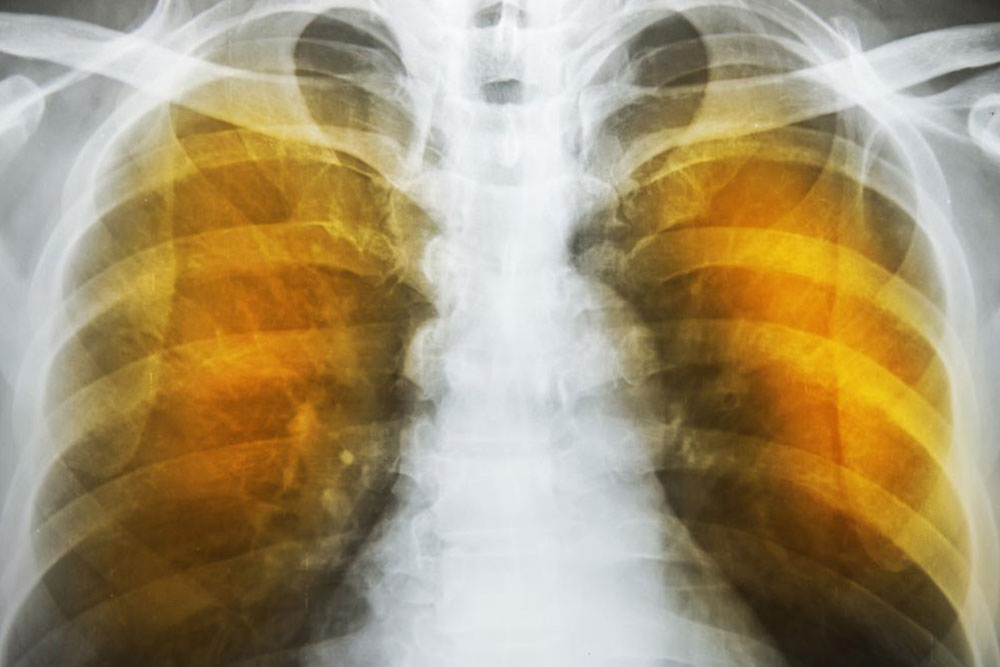
During respiration, airborne particles can settle in mucus within the airways. Individuals with bronchiectasis face difficulty in clearing this mucus due to lung tissue damage, which causes airway widening or pouch-like formations. This blockage hampers mucus clearance, raising infection risk, promoting bacterial growth, and aggravating inflammation and lung damage.
Disease Progression Stages Bronchiectasis advances through two main stages. The initial phase involves infection or inflammation damaging lung tissues, heightening vulnerability to recurrent infections and inflammation. The second stage involves sustained airway damage, leading to more severe symptoms.
The early stage increases the risk of ongoing inflammation and infections, accelerating lung deterioration. Causes of bronchiectasis vary, with up to 40% of cases stemming from unknown factors. It is often associated with conditions such as cystic fibrosis, autoimmune illnesses, and other health issues including:
Autoimmune disorders
Immunodeficiency conditions like HIV and diabetes
Inflammatory bowel diseases such as Crohn’s disease or ulcerative colitis
Allergic bronchopulmonary aspergillosis—an allergic response in the lungs
Women are slightly more prone, though men can also develop the condition
Recurrent infections, additional health problems, or airway obstructions like benign growths can also contribute. The disease can be classified by severity: cylindrical (mild), cystic (advanced), as well as focal and traction bronchiectasis resulting from lung scarring.
The condition typically develops gradually, with early signs like a persistent cough and daily mucus production. As it progresses, symptoms may include shortness of breath, fever, blood in mucus, fatigue, wheezing, nail clubbing, chest pain, and foul-smelling sputum.
Management aims to control symptoms and prevent complications. Antibiotics are prescribed based on infection severity and bacterial resistance. Additional treatments include mucus-thinning medications, inhalers, and airway clearance methods such as physiotherapy or specialized devices. Severe cases might require oxygen therapy or surgery.
Long-term care involves regular consultation with healthcare providers, maintaining a balanced diet, hydration, medication adherence, and vaccination updates. Flare-ups can still occur despite precautions, so prompt medical attention is essential for worsening symptoms like increased mucus, fever, or breathing difficulties.
Important Reminder: This content is for educational purposes only. Always seek advice from qualified healthcare professionals for diagnosis and treatment options.