A Complete Guide to Managing Diverticulitis: Causes, Symptoms, and Nutrition Tips
Learn about diverticulitis, its symptoms, causes, and effective dietary strategies. This guide covers stages of recovery, including liquid diets, low-fiber, and high-fiber foods, along with tips on probiotics and vitamin D to support intestinal health and prevent future episodes.

Comprehensive Insights into Diverticulitis: Causes, Symptoms, and Dietary Approaches
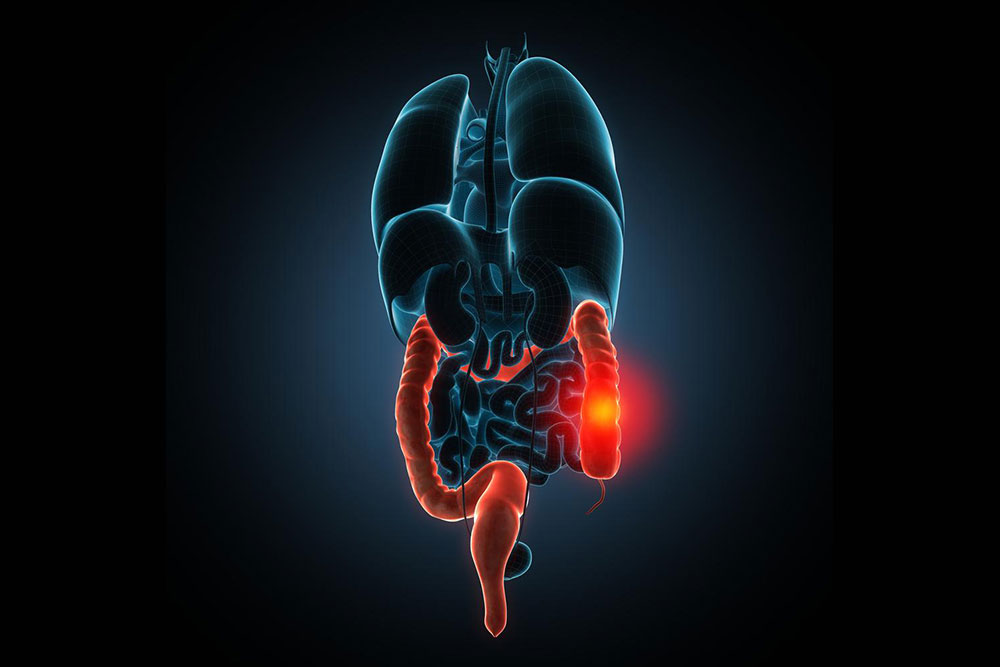
Diverticulitis is an inflammation of the colon characterized by small pouches called diverticula forming along the intestinal lining. If untreated, it can cause serious issues like abscesses, infections, or intestinal perforation, sometimes requiring surgery.
Recognizing Symptoms
Common signs include left-sided abdominal pain that often eases with bowel movements or gas. Other symptoms involve visible blood in stool, ongoing discomfort, bloating, nausea, and altered bowel habits such as diarrhea or constipation.
Timely treatment is crucial since delays can lead to complications like intestinal blockages. Severe cases may necessitate surgical procedures or blood transfusions due to bleeding.
Risk Factors and Causes
Poor diet, obesity, lack of physical activity, and smoking can increase risk. A diet low in fiber may contribute to the formation of diverticula and subsequent inflammation.
Dietary Strategies for Diverticulitis
Initially, antibiotics are prescribed to fight infection, followed by dietary adjustments to promote healing and prevent recurrence. Proper nutrition minimizes bowel strain and accelerates recovery.
Liquid Phase When symptoms flare, switch to clear fluids like water, broth, herbal teas, clear soups, fruit juices without pulp, and ice pops. Staying hydrated is vital; however, extended liquid diets may lead to weakness and need nutritional supplements.
Low-Fiber Diet As symptoms lessen, transition to foods like cooked fruits (without skins or seeds), lean meats, eggs, white rice, pasta, low-fat dairy, and refined grains. Maintain fiber below 10 grams daily initially, then gradually increase as tolerated.
High-Fiber Diet Post-Recovery After healing, aim for 25-35 grams of fiber daily from whole grains, fruits, vegetables, beans, and legumes to support colon health, prevent diverticula formation, and promote regular bowel movements. Dietary fiber adds bulk, easing stool passage.
Nuts, Seeds, and Fermented Foods Nuts and seeds contribute fiber and aid digestion, reducing future risks. Incorporate cucumber, pumpkin, sunflower, zucchini, tomato, and strawberry seeds. Fermented foods like yogurt, kefir, sauerkraut, kimchi, and miso introduce probiotics that enhance gut health and may ease symptoms.
Vitamin D Low vitamin D levels have been associated with increased diverticulitis risk. Sun exposure and supplements can help maintain healthy levels, supporting gut immunity and reducing inflammation.
Consistent hydration and a balanced, stage-specific diet encourage healthy bowel functions and lower recurrence chances. A well-functioning gut is essential to overall health.
Note:
Our blog discusses a variety of health topics with evidence-based insights. These articles are for informational purposes and not a substitute for medical advice. Consult healthcare professionals for personalized treatment options. We strive for accuracy but cannot guarantee completeness or endorse any commercial products.