Complete Overview of Herniated Disc Management and Treatment Strategies
This comprehensive guide covers herniated disc symptoms, causes, and treatment options. It highlights conservative therapies and when surgery might be needed. Early diagnosis and proper care are essential for recovery, making this resource valuable for those affected by disc herniation. Learn about managing pain, restoring mobility, and preventing future issues effectively.
Understanding Herniated Discs: Symptoms, Causes, and Treatment Options
Herniated discs can lead to numbness, weakness, or tingling sensations in one or both legs. This occurs when the soft core of an intervertebral disc protrudes through its outer layer. While some cases may not be painful or cause rupture, timely treatment is crucial for symptom relief. These discs most often affect the neck (cervical), upper/mid-back (thoracic), and lower back (lumbar).
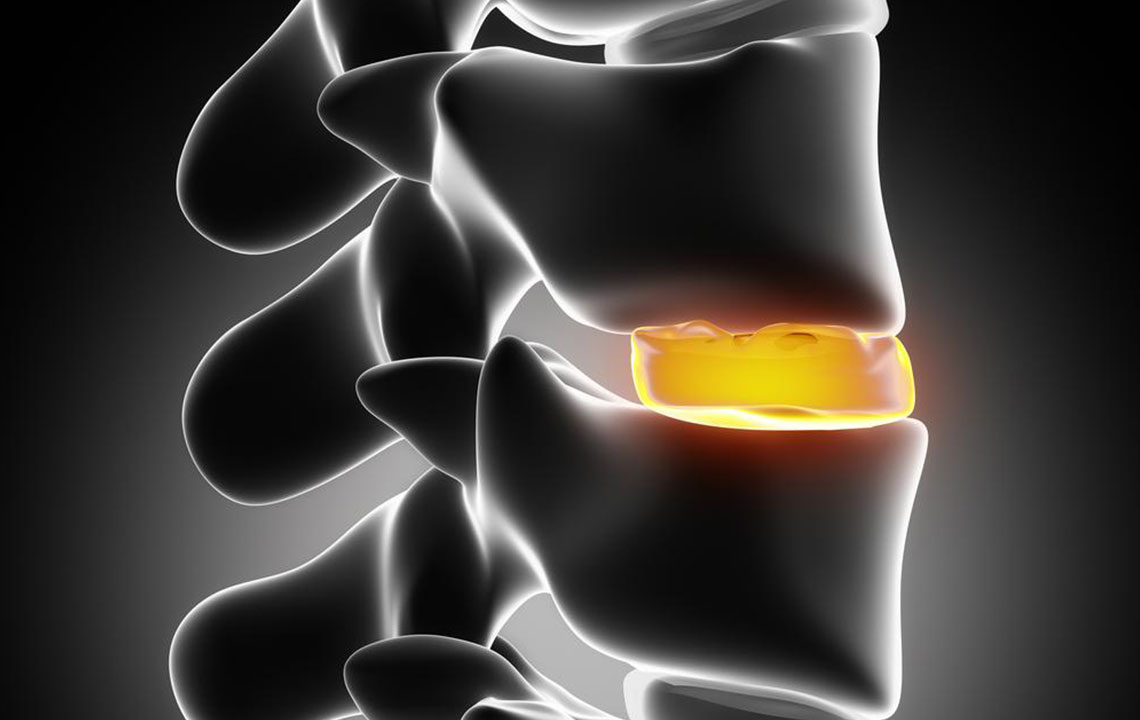
Intervertebral discs serve as shock absorbers between vertebrae, composed of a gel-like nucleus encased in a fibrous ring called the annulus. Damage to this outer layer allows the inner material to protrude, compressing nearby nerves and causing pain. Herniations can range from minor bulges to full ruptures, often due to weakened disc walls or sudden trauma. Repetitive stress, impact, or genetic factors may increase the risk.
Nerve compression from herniated discs often results in numbness, muscle weakness, spasms, and pain. Symptoms vary based on the disc location:
In the thoracic region: numbness, leg weakness, reflex changes, potential bowel or bladder issues, and paralysis below the waist.
In the cervical area: neck pain, shoulder discomfort, radiating pain into arms and fingers, and limited mobility.
Symptoms usually develop gradually but can worsen with activity. Accurate diagnosis through imaging is essential for effective treatment.
Common Treatment Approaches for Herniated Discs
Initial management typically involves conservative, nonsurgical methods. Treatment progress through phases:
Phase 1: Pain Relief and Inflammation Control — Using ice, electrotherapy, or acupuncture.
Phase 2: Restoring Flexibility and Strength — Targeted exercises to enhance mobility and core stability.
Phase 3: Resuming Activities — Gradual return to walking or light activities based on individual tolerance.
Phase 4: Prevention — Daily routines to avoid future herniation and promote spinal health.
If symptoms persist despite conservative treatments, surgical options may be considered. The choice of surgery depends on herniation severity and location. Early intervention can help prevent long-term issues. Always consult a healthcare professional for a personalized plan.


